Introduction
Menopause marks a major turning point in a woman’s life — emotionally, hormonally, and physically. While hot flashes and mood swings often get the spotlight, one silent yet significant change happens beneath the surface — bone loss.
The drop in estrogen levels during menopause directly impacts bone density, increasing the risk of osteopenia and osteoporosis. But here’s the good news — through mindful lifestyle choices, women can preserve bone strength and prevent fractures well into their later years.
This blog explores how menopause affects bone health, the warning signs of bone loss, and most importantly, what you can do daily to protect your bones naturally.
Understanding the Link Between Menopause and Bone Loss
Estrogen isn’t just a reproductive hormone — it also plays a vital role in maintaining bone strength. It helps regulate the process of bone remodeling, where old bone tissue is replaced with new, strong bone.
When estrogen levels plummet after menopause (usually between ages 45–55), the balance between bone resorption (breakdown) and bone formation shifts. The body begins losing bone faster than it can rebuild it.
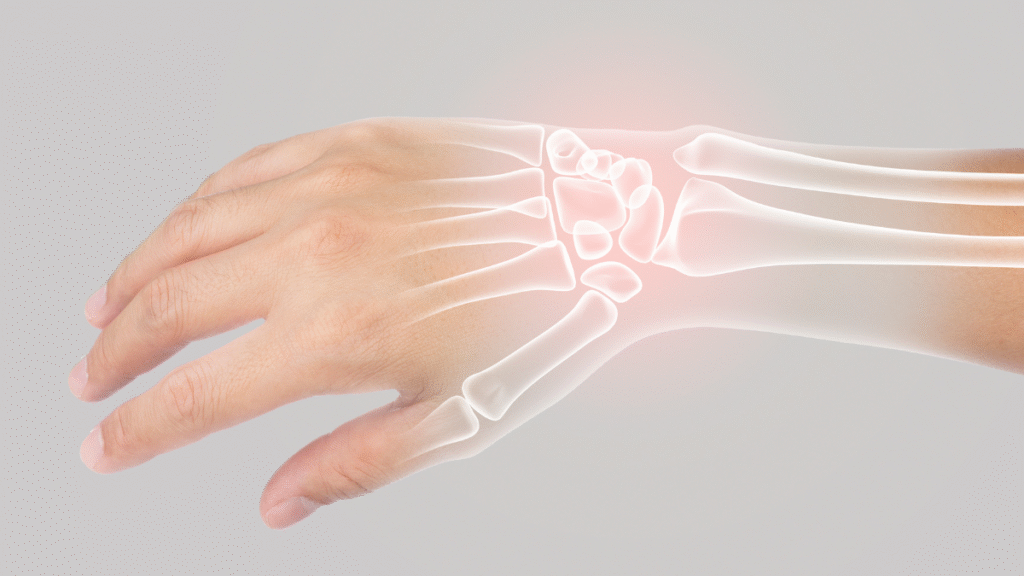
Studies show that women can lose up to 20% of their bone density in the 5–7 years following menopause. This rapid bone loss significantly increases the risk of fractures, especially in the spine, hips, and wrists.
Signs You Might Be Losing Bone Density
Bone loss is often called the “silent thief” because it progresses without obvious symptoms until a fracture occurs. However, a few subtle signs may indicate weakening bones:
- Loss of height over time
- A stooped or hunched posture
- Back pain from vertebral fractures
- Fragile bones that break easily
If you’re postmenopausal, it’s essential to get a bone density test (DEXA scan) to assess your bone strength and risk level.
Top Lifestyle Choices to Prevent Osteoporosis After Menopause
1. Prioritize Calcium and Vitamin D
Calcium is the foundation of strong bones, while vitamin D helps your body absorb it effectively.
- Calcium-rich foods: Dairy products (milk, cheese, yogurt), tofu, sesame seeds, sardines, broccoli, and fortified plant milks.
- Vitamin D sources: Sunlight (10–15 minutes daily), egg yolks, fatty fish, and fortified foods.
Tip: Postmenopausal women generally need 1,200 mg of calcium and 800–1,000 IU of vitamin D daily. Supplements can help fill nutritional gaps when diet alone isn’t enough.
2. Engage in Weight-Bearing and Strength Training Exercises
Physical activity is one of the most powerful ways to preserve bone mass. Weight-bearing exercises put healthy stress on the bones, stimulating them to stay strong.
- Weight-bearing exercises: Walking, jogging, stair climbing, hiking, dancing.
- Strength training: Lifting weights, resistance bands, Pilates, or bodyweight exercises (like squats and lunges).
Consistency matters — aim for at least 30 minutes of weight-bearing activity most days and 2–3 strength sessions per week.
3. Maintain a Balanced Diet
A diet rich in bone-supporting nutrients helps protect against bone loss.
Include foods rich in:
- Magnesium: Leafy greens, nuts, and seeds
- Vitamin K: Spinach, kale, and broccoli
- Protein: Essential for bone repair — opt for lean meats, lentils, and Greek yogurt
- Omega-3 fatty acids: Found in salmon, walnuts, and flaxseeds, these healthy fats may reduce bone inflammation
Avoid excessive salt, caffeine, and alcohol, as they can cause calcium loss from bones.
4. Manage Menopausal Stress
Chronic stress raises cortisol, a hormone that can accelerate bone loss by interfering with calcium absorption. During menopause, stress often compounds the effects of low estrogen.
Incorporate stress-reducing practices such as:
- Meditation or deep-breathing exercises
- Yoga or tai chi (which also improve balance and prevent falls)
- Spending time in nature
- Journaling or mindfulness practices
5. Quit Smoking and Limit Alcohol
Smoking speeds up bone loss by affecting estrogen production and calcium absorption.
Similarly, excessive alcohol intake interferes with vitamin D metabolism and weakens bones over time.
Moderation tip: Keep alcohol to no more than one drink per day, and if you smoke, consider a structured cessation program.
6. Hormone Replacement Therapy (HRT) — A Medical Option
For women experiencing rapid bone loss or early menopause, Hormone Replacement Therapy (HRT) can help maintain bone density by replacing declining estrogen levels.
However, HRT isn’t suitable for everyone and may carry certain risks. Discuss this option thoroughly with your gynecologist or endocrinologist before starting any therapy.
7. Regular Checkups and Screening
After menopause, schedule routine bone density scans every 2 years to monitor bone health.
Also, discuss with your doctor whether medications such as bisphosphonates, selective estrogen receptor modulators (SERMs), or parathyroid hormone analogs are appropriate for you if you have diagnosed osteoporosis.
Holistic Bone Health: Beyond Diet and Exercise
Bone health isn’t just physical — it’s emotional and energetic too. Emotional well-being plays a subtle role in hormonal balance.
Mind-body practices like mindfulness, restorative yoga, and gratitude journaling can support your nervous system, which indirectly benefits your bones through better stress regulation and improved sleep quality.
Conclusion
While menopause naturally increases the risk of osteoporosis, it doesn’t have to mean frailty or fractures.
By adopting bone-nourishing habits — from a calcium-rich diet and regular exercise to stress management and routine screenings — women can build resilience from the inside out.
Your postmenopausal years can be strong, active, and vibrant — it’s never too early (or too late) to start taking care of your bones.
FAQs on Bone Health After Menopause
1. When should women start worrying about bone health?
Bone density begins to decline in your mid-30s, but after menopause, the rate increases sharply. It’s best to start preventive steps early — even before menopause.
2. Can I rebuild lost bone after menopause?
While you can’t fully reverse bone loss, lifestyle changes, medication, and exercise can significantly slow down or stabilize the process.
3. Is dairy the only good source of calcium?
No. You can get calcium from plant-based sources like almonds, tofu, sesame seeds, broccoli, and fortified non-dairy milks.
4. How does yoga help bone health?
Yoga improves balance and flexibility, which helps prevent falls — a major cause of fractures in older women. Certain poses also apply mild stress to bones, stimulating growth.
5. Can vitamin D deficiency worsen bone loss?
Absolutely. Without enough vitamin D, your body can’t absorb calcium properly, leading to brittle bones and higher fracture risk.