Introduction
Many women notice something puzzling during their 40s and 50s — even with a balanced diet and regular exercise, their blood sugar levels, especially in the morning, start to rise unexpectedly. This isn’t a coincidence. It’s a direct result of the hormonal shifts that occur during menopause.
Menopause brings profound changes to the body’s metabolism, insulin sensitivity, and stress response — all of which can contribute to higher fasting blood sugar and more frequent glucose spikes. Understanding why this happens is the first step toward managing it naturally and effectively.
In this blog, we’ll explore why morning blood sugar becomes harder to control after 40, how menopause impacts glucose metabolism, and practical steps you can take to stabilize your levels and feel more energetic throughout the day.
Understanding the Link Between Menopause and Blood Sugar
During perimenopause and menopause, estrogen and progesterone — two key female hormones — begin to fluctuate and eventually decline. These hormones do much more than regulate menstruation; they also play a vital role in how the body processes insulin and glucose.
Here’s how the hormonal connection works:
- Estrogen helps cells absorb glucose from the blood and use it for energy. When estrogen levels drop, the body becomes less sensitive to insulin, meaning glucose stays in the bloodstream longer.
- Progesterone affects appetite, sleep, and mood — all of which can indirectly influence blood sugar regulation.
- As both hormones fluctuate unpredictably, blood sugar stability is disrupted, leading to sudden spikes and crashes.
This hormonal roller coaster makes it much harder to maintain steady glucose levels — particularly first thing in the morning, when hormones naturally shift again.
Why Morning Blood Sugar Levels Spike After 40
If you’ve ever checked your blood sugar in the morning and found it higher than expected, even after a healthy dinner, you’re not alone. This phenomenon is often linked to something called the “dawn phenomenon.”
1. The Dawn Phenomenon
In the early morning hours (typically between 2 a.m. and 8 a.m.), the body releases hormones like cortisol, glucagon, and growth hormone to prepare for the day ahead. These hormones tell the liver to release glucose into the blood for energy.
In younger women, estrogen helps regulate this process. But after 40, declining estrogen levels make the body less efficient at controlling this glucose release, leading to higher fasting blood sugar levels.
2. Reduced Insulin Sensitivity
Menopause often brings insulin resistance, meaning the body doesn’t use insulin as effectively as before. This causes glucose to accumulate in the bloodstream, particularly overnight.
3. Stress and Cortisol Overload
During menopause, cortisol (the stress hormone) levels can remain chronically elevated due to sleep disruptions, anxiety, and hormonal imbalance. High cortisol increases glucose production by the liver, further driving morning spikes.
4. Sleep Disturbances
Hot flashes, night sweats, and insomnia are common during menopause and lead to poor-quality sleep. Lack of deep rest triggers hormonal imbalance and increases insulin resistance, causing higher fasting glucose levels the next morning.
5. Slower Metabolism
With age and hormonal decline, metabolic rate naturally slows down. This means the body takes longer to process glucose, and fasting levels may stay elevated for longer periods.
Symptoms of Blood Sugar Imbalance During Menopause
Fluctuating blood sugar often shows up as subtle daily symptoms. Some women experience:
- Cravings for sweets or carbs
- Midday energy crashes
- Irritability or mood swings
- Difficulty concentrating (“brain fog”)
- Unexplained fatigue
- Weight gain around the abdomen
If these sound familiar, it may be time to monitor your blood sugar patterns — especially your fasting readings.
How to Naturally Manage Blood Sugar During Menopause
While these changes are normal, you can take several steps to regain control of your blood sugar and overall well-being.
1. Prioritize a Balanced Breakfast
Skipping breakfast or eating sugary cereals can worsen morning spikes. Instead, opt for a protein- and fiber-rich meal that stabilizes glucose levels — such as eggs with vegetables, Greek yogurt with chia seeds, or a smoothie with protein powder and healthy fats.
2. Reduce Refined Carbohydrates and Sugar
Refined carbs (white bread, pastries, pasta) and sugary snacks cause rapid glucose spikes. Choose whole grains, lentils, and low-glycemic fruits instead to support sustained energy release.
3. Stay Hydrated
Dehydration can raise blood sugar levels. Drink water throughout the day and limit sugary drinks or excess caffeine.
4. Manage Stress
Chronic stress elevates cortisol, which triggers glucose release. Practice stress-relieving activities like meditation, yoga, or deep breathing to calm your nervous system and lower cortisol naturally.
5. Exercise Regularly
Physical activity increases insulin sensitivity and helps muscles absorb glucose efficiently. Combine strength training (to counter muscle loss) and aerobic exercises like walking, swimming, or cycling for optimal results.
6. Prioritize Sleep
Aim for 7–8 hours of uninterrupted sleep. A relaxing bedtime routine, a cool room, and limiting screen time can help minimize sleep-related glucose fluctuations.
7. Consider Magnesium and Omega-3-Rich Foods
Magnesium helps improve insulin sensitivity, while omega-3 fatty acids reduce inflammation. Include foods like nuts, seeds, fatty fish, and leafy greens in your diet.
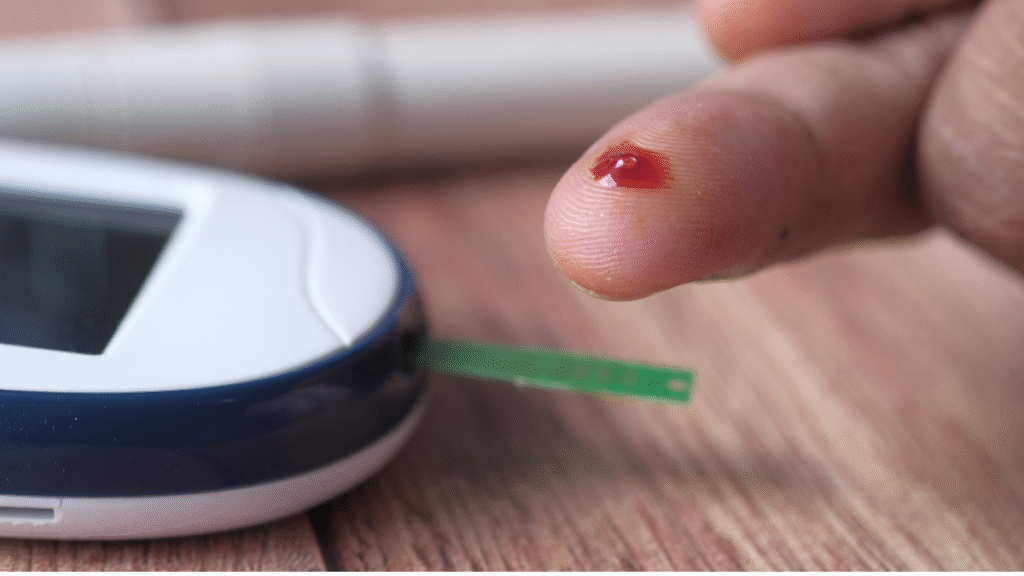
8. Track Your Blood Sugar
If possible, use a Continuous Glucose Monitor (CGM) or a home glucose meter to observe how your body responds to different foods, stress levels, and sleep patterns. Tracking empowers you to make data-driven lifestyle adjustments.
When to Consult a Healthcare Professional
If your fasting blood sugar remains consistently high (above 100 mg/dL) or you experience symptoms like frequent thirst, fatigue, or blurred vision, consult your doctor. They may recommend blood tests to check for prediabetes or diabetes, and help tailor a personalized plan that may include diet, exercise, and medication if needed.
Reclaiming Balance After 40
Menopause is not just a hormonal transition — it’s a metabolic one. Understanding how these changes affect your blood sugar gives you the power to take proactive steps toward better health.
By eating mindfully, managing stress, staying active, and supporting your hormones naturally, you can stabilize your blood sugar and prevent the midlife energy crashes that so many women experience.
Remember: menopause is not an end — it’s an opportunity to reset your health and strengthen your relationship with your body.
Conclusion
Blood sugar spikes during menopause are a common yet manageable issue. The hormonal decline after 40 — particularly reduced estrogen and progesterone — directly affects insulin sensitivity, stress levels, and glucose metabolism. Morning blood sugar levels become harder to control because of the dawn phenomenon, hormonal shifts, and stress-related cortisol surges.
But with mindful eating, stress management, good sleep, and regular movement, women can regain balance naturally. Taking control of your metabolic health during menopause isn’t just about blood sugar — it’s about feeling strong, calm, and energized for the next chapter of your life.
FAQs
1. Why are my fasting blood sugar levels high even though I eat healthy?
Hormonal fluctuations during menopause can cause insulin resistance, which makes your body less efficient at using glucose — even if your diet is balanced.
2. What is the dawn phenomenon in menopause?
It’s an early-morning rise in blood sugar caused by hormones like cortisol and glucagon. With lower estrogen levels after 40, your body finds it harder to regulate this glucose release.
3. Can menopause cause diabetes?
Menopause itself doesn’t cause diabetes, but it increases the risk of insulin resistance and prediabetes. Lifestyle changes can significantly lower this risk.
4. Does hormone replacement therapy (HRT) affect blood sugar?
Some studies show HRT can improve insulin sensitivity, but it’s not suitable for everyone. Always consult your doctor before starting or stopping HRT.
5. Can meditation or yoga help control blood sugar during menopause?
Yes. Both reduce stress hormones and improve metabolic function, helping to keep blood sugar levels more stable.